The Season of Sneezing

It’s once again time to run my annual column on allergies. Some of our readers may already cursing the annual return of allergy symptoms. Tree pollen levels (Oak, Cedar/Juniper, Nettle) in Indiana have been high recently. Spring allergy symptoms can make it even more difficult to differentiate who might have lingering COVID-19 symptoms or just run of the mill allergy symptoms.
Seasonal allergies are a major problem for many people. When allergy sufferers are asked about their quality of life, they generally rate allergies as more bothersome than heart disease and sometimes even cancer. Many different things cause allergies; I want to focus on the seasonal type.
Seasonal allergies are caused by pollen. Pollen contains the male genetic material of plants; it is analogous to sperm in animals. The key to survival of any biologic organism is to disseminate its genes as far and wide as possible to combine with that of others in the species. Pollen is an exquisite vehicle to accomplish this task.
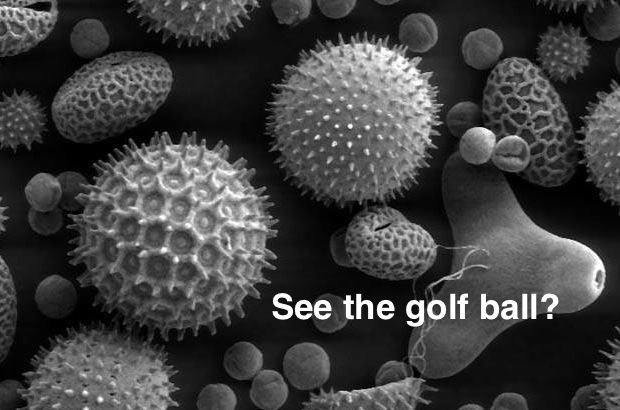
There are two main categories of pollen – anemophilous (wind-loving) and entomophilous (insect-loving). Anemophilous pollen is very lightweight which allows it to move great distances, particularly on windy days. Anemophilous pollen is produced by trees, grasses and weeds. Golf ball engineers have used biomimicry of pollen grains to design the dimples on the balls to allow them to fly farther.
Entomophilous pollen is produced primarily in plants that bear flowers. It is much heavier and stickier, allowing it to be picked up and spread by insects such as bees. The loss of pollinating insects due to things like insecticide use and climate change is a real threat to these types of plants. Entomophilous pollens are much less likely to cause allergies since they are not typically inhaled or blown into noses by the wind.
Plants produce and release pollen at various times of the year, hence the seasonal nature of allergies. Trees in Indiana start pollinating in late February and usually end sometime in May. Each species of tree pollinates for around one to two weeks.
Grasses start pollinating in April and continue through May. Hoosiers then get a little break until about mid-August when ragweed starts up and continues until sometime in October. The allergy season has become longer over the past two decades, starting two to three weeks earlier and lasting two to three weeks longer. This is very likely due to warming from climate change.
Pollen grains contain proteins on their surfaces that attach to the tissues on the inside of the nose. In order to develop allergies, a person’s immune system must be genetically programmed to recognize these proteins as foreign invaders. This occurs in about 40 percent of people.
A person’s immune system reacts to these proteins by creating a specific class of antibodies called immunoglobulin E (IgE). The process of developing IgE in sufficient quantities to cause problems can take anywhere from two to ten years. This is why people often don’t develop allergies until they have been exposed to an allergen for a number of years (the family dog’s skin dander for instance).
When IgE is produced it attaches to the surface of specialized mast cells where it sits, waiting to do its job. When pollen finds its way to a mast cell coated with IgE programmed to react to it, it binds to the IgE and causes the cell to release various substances that cause allergy symptoms.
One of the most common molecules released by mast cells is histamine. It causes the typical nasal symptoms of congestion and watery discharge as well as red, itchy, watery eyes, and perhaps wheezing. These physical effects are all designed to do one thing – cough, sneeze, or flood the allergen out of the body.
Diagnosing pollen allergies is fairly straightforward. The offending agent can often be determined based on the time of year a patient develops symptoms. Sometimes the services of an allergist are required to do skin or blood tests to identify the specific offender(s).
There are numerous treatments for allergies. Avoidance is the most important prevention strategy – stay indoors when possible, particularly on windy days, and run the air conditioning instead of opening windows. Saline (salt water) rinses can be very effective at rinsing pollen out of the nose. This can be done using commercial products such as a Neti Pot or squeeze bottle such as Sinus Rinse® manufactured by NeilMed.
Antihistamines are also a mainstay of treatment. These medications block the release of histamine by mast cells. There are numerous antihistamines available both off the shelf and by prescription. Older antihistamines like Benadryl® (diphenhydramine) often cause drowsiness, but remain very effective. Newer medications like Claritin® (loratadine), Allegra® (fexofenadine), Zyrtec® (cetirizine) and XYZAL® (levocetirizine) are generally less sedating but tend to be a bit more expensive.
Other treatments are also available such as nasal steroid sprays like Flonase® (fluticasone) and sprays to prevent mast cells from releasing histamine. Severe allergy sufferers, or those who fail other therapies, may need to move on to allergy injections under the skin or drops under the tongue to reduce the severity of allergy symptoms.
– Dr. John Roberts is a member of the Franciscan Physician Network specializing in Family Medicine as well as the Deputy County Health Officer in Montgomery County.
